By Dr. Wayne Ruga, FAIA, FIIDA, Hon. FASID
This article is about the future – yours, mine, and everyone’s. It is a ‘call’ to courageous progress.
Background: The expression, ‘crossing the Rubicon’, is meant to evoke a decision to a significant course of action – an irrevocable action where there is no going back, as in 49 BC, when Julius Caesar crossed the Rubicon River and the events leading to the rise of the Roman Empire unfolded. In the 1970s, Thomas Kuhn developed the concept of a ‘paradigm shift’, with a similar meaning. Today, it is common to hear the expression, ‘let’s get out of the box’, a metaphor meaning much the same. In all three of these cases, radical progress is harkened – a systemic improvement over the status quo – one that requires courage to advance into the ‘beyond’.
At the 2017 30th annual Symposium, in Austin, we commemorated this milestone event by drawing upon the image and legend of Janus – the Roman god of transitions. The image portrays Janus as a left and a right profile – with a straight-on portrait between these two profiles – to mean that, as we progress into the future, we should inform our journey with learnings from the past. At the 30th Symposium, as we discussed progressing into a future informed by learnings from the past, none of us could have imagined the arrival of the Pandemic on our doorstep, about to challenge everything we thought we knew.
Foreground: As we make our preparations to return to Austin for this year’s 2021 Symposium – having completely skipped a Symposium for the first, and only, time in the history of the event – to be certain, during the last 20 months, we have all been required to cross the Rubicon, shift numerous paradigms, and get ourselves out of many a box. In my roles as the Symposium founder, healthcare and design innovator, pioneer of new futures, and teacher, I am frequently asked to comment on what we’ve learned through the challenges of this pandemic that will have a lasting, positive impact on how we create our future.
In this regard, the Sankofa – the mythical bird of Ghana – offers useful guidance. It is an inspired legend that reminds us of Janus, with the additional dimension of ‘wisdom’. The native Akan tribe, the source of the Sankofa legend, believe that the past should guide us in how we plan our future – and, that it is the wisdom from this learning that enables us to make a stronger future likely. In the tradition of Socrates – I turn the question to you: what have you learned during these 20 months, what wisdom have you gained, and how will this wisdom inform the decisions you will make as you progress into the new future?
My own view on this question – what have we learned – has multiple dimensions: (1) how can the Symposium impact the new future; (2) what impact can I (the collective ‘I’) possibly have on the new future; and (3) how can ‘I’ contribute – positively – toward creating a new, and better, future? How each one of us addresses these dimensions is profoundly crucial, in terms of how our collective new future will unfold.
For example: How can the Symposium impact the new future? First-time attendees may get the impression that the Symposium is a conference – although it contains many of the same elements that a conference does, it has so much more to offer. The Symposium can be better understood as a crucible, a vessel where transformation is forged. Each year, radically new ideas are presented and discussed that are carried by the attendees further into the world to advance progress. Whether these ideas exist as information, knowledge, or wisdom – it takes courage to learn new ideas and use them to improve the status quo, as Symposium attendees have done for decades, as inspired and courageous agents of transformation in health and healthcare.
The Symposium, as a crucible, has an established pioneering legacy of fueling the transformation of the individual lives of its attendees by providing direct exposure to: new, and often – very different – ways of thinking; new connections, support, and resources from meeting and engaging with like-minded individuals; and new business opportunities. There is no other healthcare facilities design event that has so profoundly improved lives around the globe, because of this transformative function – the lives of patients, families, staff, and local community residents.
To find ourselves asking, ‘what impact can I possibly have’ is to overlook the many unique opportunities that have opened up because of this unprecedented moment in our history. Every single individual has a significant, unique, contribution to make towards the creation of a new and better future – although it is not always so easy to see that, and to have a clear idea of what we each can do. This is precisely why we must reach into the ‘beyond’ – the beyond the Rubicon, into the new paradigm, and get ourselves out of the box. As Hillel the Elder said. ‘If not now, when? If not you, who?’. Now is the time.
The question: ‘how can I contribute – positively – towards creating a new and better future?’ is not a simple question with a simple answer. It is an inquiry that each one of us has the opportunity – and responsibility – to engage in. Why do I make this bold assertion that we each have the ‘responsibility’ to consider this question? My view is that we are all leaders – some of us are highly visible and recognized leaders, with ‘leader’ written in all capital letters; many more of us are leaders, written simply with a capital ‘l’; and – most importantly – every single one of us is a leader in lower case letters: the leader of an enterprise, called ‘my life’. As the leader of this personal enterprise, we are the CEO, and we have sole leadership responsibility – as the CEO of our life – just as the CEO of a major organization has. In this role, we have the responsibility to discover how our inherent personal, unique, agency can find purchase – and traction – to advance our own enterprise.
Of course, advancing our enterprise does not necessarily mean that we will contribute positively towards creating a new and better future – so, I qualify my comments by drawing upon the words of Reinhold Niebuhr, author of the ‘Serenity Prayer’: ‘God, grant me the serenity to accept the things I cannot change, courage to change the things I can, and wisdom to know the difference’. From this prayer, I highlight the words, ‘courage’ and ‘wisdom’. The Sankofa enabled us to appreciate the value of wisdom in informing our future with learnings from our past – a new understanding that the teachings of Janus were silent on.
‘Courage’, however, is a new aspect – one that the Serenity Prayer contributes to our inquiry: a personal exploration of considering what things can I actually change? In our modern times, definitions and understandings of ‘courage’ have emphasized brave and fearless actions, particularly when faced with adversity. Examining the origins of ‘courage’ provides us with a further understanding – ‘courage’ is derived from the Latin root of ‘cor’: of the heart. When ‘courage’ is used in this original way, it encourages us to discover and to speak openly of truths from our heart, as opposed to brave and fearless actions, which have their origins in our brains.
As we further consider the root of ‘courage’, we must each discover a personal way to understand our heart in a new way – not merely as a mechanical pump for the purpose of circulating blood, but – rather – as the center for our ability to gain access to unique intelligences that – amongst their far-reaching capacities, enables each one of us to pursue courageous self-expression. Neibuhr’s Serenity Prayer invites us to use our ‘wisdom to know the difference’ – a profound opportunity to learn how to clearly distinguish the wilful volition of brain-driven actions, from the more subtle and elusive callings of our hearts, and – as a result – access personal expressions of ‘courage’ that can move mountains and transform futures.
What have we learned? If it isn’t as obvious to you as it is to me – old habits are hard to change, and ‘necessity is the mother of all invention’. It is surprisingly easy – more than we imagined – to try doing old things in new ways, and – presto – the outcomes are improved. What about making a really big stretch, and also discovering how to do new things in new ways?
The September / October 2021 issue of Harvard Magazine has a feature article, ‘The State of the Pandemic: Lessons Learned from the Continuing Confrontation with the Virus’. It discusses a range of lessons learned – some of which call to us to create futures that – heretofore – were unimaginable. For example, the article reminds us that the Pandemic is a global challenge, and we have not yet developed the global structures to adequately withstand future health threats – or the resources. In our current era, the wealthiest countries can have the best outcomes, while our less wealthy relatives have less robust defences – is this the future we really want for our children, and their children?
The article mentions the built environment, and some of the health challenges that our current inventory provides – such as closed and ventilated buildings, and insufficient intensive care capacity for future epidemics. As a community of leaders, with a passionate interest for improving health and healthcare facilities, we can expect that the Symposium will inspire novel remedies to these deficiencies that will contribute towards improving the resilience that we rely on our essential services to have, and to continuously upgrade.
A ‘Call to Courageous Progress’: Pablo Picasso famously said, ‘I am always doing that which I cannot do, in order that I may learn how to do it.’ No doubt, if Picasso was still alive, he would have been a notable Symposium Keynote speaker, and a regular attendee. Although the richness of the distinctly different Symposium attendees is invigorating, Picasso’s quote provides a fascinating snapshot of the key characteristics that weave their way through the global Symposium community – a commitment to regularly and consistently doing the impossible, and continuous learning. And, as a Picasso scholar might explain to us, Picasso’s quest to be ‘always doing that which I cannot do’ was driven by his courage – in translating the wisdom of his heart and learning to create from this source – much as each one of us might do, as we courageously progress on our respective leadership journeys, in creating a new and better future for the many generations to come.
In conclusion, this ‘call’ is a thundering shout: now is the time to draw a line in the sand, beyond which is a new and much better future than our recent past (50 years?). Let’s all discover and draw from our wisdom, learn from our journey, and invest our precious life force into courageous demonstrations of our unique agency – the gifts we were born with, the legacy that our ancestors bequeathed to us, and the dreams that inspire each one of us to leave this world better than when we arrived.
Wayne Ruga can be reached at: [email protected].







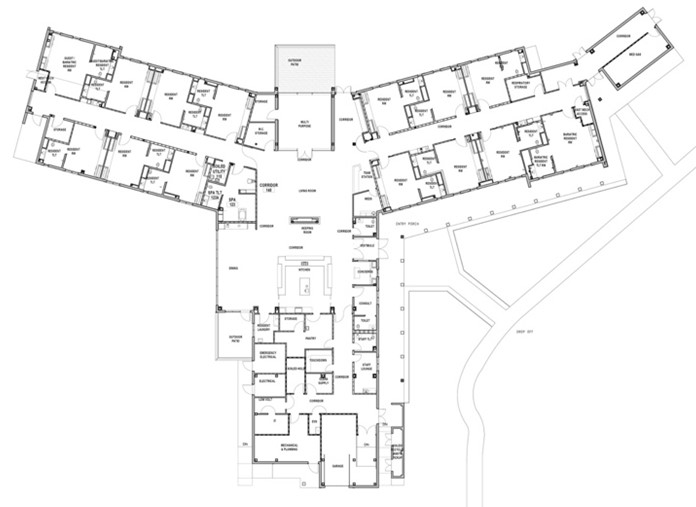
 In 2019, the Lebanon, PA Veterans Affairs (VA) Medical Center tapped Miller Remick and Array Architects to design and construct a Community Living Center (CLC) that follows the VA standard small house modelfor their campus. Little did the team know that the pandemic was about to fundamentally change how age-in-place environments are designed. In this article, we’ll review strategies to adapt existing designs to meet new guidelines by exploring how the design team addressed MEP and operational challenges posed by the pandemic.
In 2019, the Lebanon, PA Veterans Affairs (VA) Medical Center tapped Miller Remick and Array Architects to design and construct a Community Living Center (CLC) that follows the VA standard small house modelfor their campus. Little did the team know that the pandemic was about to fundamentally change how age-in-place environments are designed. In this article, we’ll review strategies to adapt existing designs to meet new guidelines by exploring how the design team addressed MEP and operational challenges posed by the pandemic. Phase one of this project consisted of a full master plan to move their current beds into
Phase one of this project consisted of a full master plan to move their current beds into